Ever since the first pacemaker was implanted into a human body back in 1958, the use of medical devices has grown to the point where it is now a routine affair. In Canada, there were over 700,000 surgeries to implant some kind of device into a patient in 2018-19. And in the US, it is estimated that as many as 10% of Americans have some kind of medical device implanted in their body. With our society aging and requiring things like hip and knee replacements, this trend is set to continue.
Although implants may have become an everyday operation, inserting foreign objects in the body is not without risks. Infections, inflammations, blood clots – the list of potential complications is long, and the rate of these occurrences is far from zero. Indeed, some observers say the rate of fatalities due to medical implant failures is so underreported that it is actually the leading cause of death in the US. One of the drivers for such failures is the body’s own response.
With this dynamic in the background, a growing trend in medical science is biocompatibility, which emerged as a concept in 1970. While many devices are termed to be “inert” and do not react to substances such as blood, the body may still not see them as being natural and provoke a detrimental response. Hence, there is a growing focus on how these items are coated to make them more biocompatible.
One recent spinoff to emerge from the McGill Innovation Fund (MIF) program is Capcyte Biotherapeutics, a team devoted to creating a coating for devices that enhances not only their biocompatibility, but also hemocompatibility (i.e., improving the interaction with blood cells), to help promote cellular regeneration. In other words, not only do they aim to have devices more readily accepted by the body, they will actually heal faster.
Finding the light of day
The project originated in the laboratory of Chemical Engineering Professor Corinne Hoesli, who has long explored the complexities of cellular interactions. She has also long been passionate about helping her technology move out of the lab and into the world where it can have an impact.
“I want the technologies that we developed in our lab to see the light of day,” Professor Hoesli explained. “I find it very rewarding to interact outside of academia.”
The team that leads Capcyte is made up of her students: Hugo Level (CEO), Marc-Antoine Campeau (CTO) and Mariève Boulanger (CFO). “Towards the end of my PhD, when Corinne approached me to do this new project where it was not just about academia but also a business opportunity of going forward and outside academia, that was really appealing to me,” said Campeau. “I didn't see myself going into academia, I wanted something else.”
One of the first applications the team examined is that of coronary stents. Coronary stents are widely used in modern medicine, with an estimated market size of $5.91 billion USD in 2019, more growth is expected in the coming years. But the nature of stents has not changed dramatically since their development in the early 1980s. And despite how commonly they are used, stents often have complications, including restenosis and thrombosis, both of which can necessitate a second procedure.
 Hugo Level explained: “Coronary stents are everywhere and even though the technology has evolved a lot since the creation of stents, we still have a significant rate of implant failure within 5 to 10 years after implementation.”
Hugo Level explained: “Coronary stents are everywhere and even though the technology has evolved a lot since the creation of stents, we still have a significant rate of implant failure within 5 to 10 years after implementation.”
“This means that the patients will need to undergo another intervention and it can be once, twice, three times. And that's a huge burden for the patient which comes from the lack of biocompatibility in a general term,” he added.
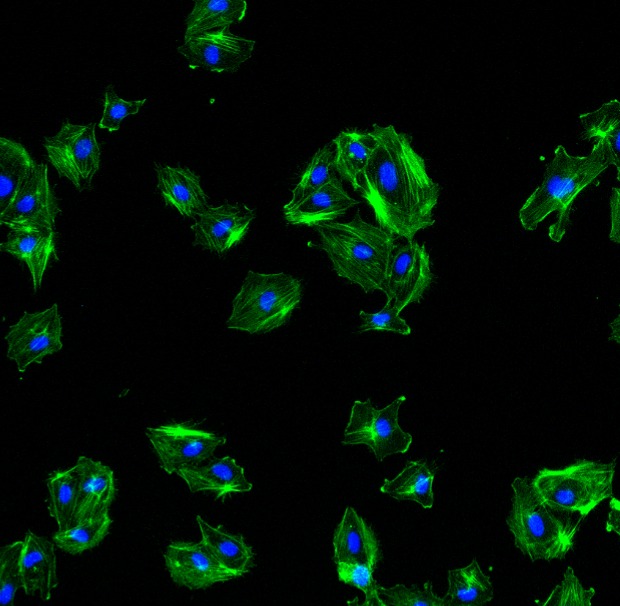
This lack of biocompatibility can be remedied by the application of Capcyte’s platform technology on the stents to improve cell interaction. Their proof of concept on coronary stents showed the benefits of their technology which include a more efficient vascular regeneration and improved hemocompatibility.
“What really differentiates Capcyte from others,” clarified CTO Campeau “is that instead of suppressing any interaction with the cells, making sure there is no clot forming, etcetera. We see the upside. We want to invite the right cells on the surface to drive the regenerative process; this is quite different from the competition.”
“We're taking materials that cells do not like, and not only do we select which cells will interact with the surface, but we do it in a way that the cells will thrive,” explained Professor Hoesli. “And that selected interaction is the common ground of the technology.”
The MIF and the Future
 The team applied to the McGill Innovation Fund’s first cohort in 2021 but was not awarded. However, they tried their luck again in 2022 and were successful.
The team applied to the McGill Innovation Fund’s first cohort in 2021 but was not awarded. However, they tried their luck again in 2022 and were successful.
“In 2021, and at that stage we weren't ready to convince the jury that we had something very strong,” admitted Level. “This time we were ready to show what impact we could have and how we could have a real competitive edge in that environment so that’s when our journey with the MIF began.”
Since then, they have been supported by the MIF’s funding and the guidance of its experts. “We are engineers, we tend to be sometimes narrow minded when it comes to business,” said Level. “We have an idea about what the technology should be and how it should work. But these mentors are really helping us to understand what would be required from an entrepreneurship point of view.”
The team is looking for clinical partners and investors to develop implants that incorporates their platform technology. “We envision creating partnerships with implant manufacturers. What we can do is to improve the surface of existing implants to make them more regenerative which means less complications for patients,” described Campeau. “So we believe we will be able to have an impact on those products that will then translate into a better treatment for the patient.”
The technology has been in development since 2015 and the team looks forward to its potential commercialization.
“One of the things that I would really like to see is an implant with our technology on it, go to clinical trials and eventually see a patient getting this implant. That would be a huge achievement because it's the core of our motivation,” concluded Level.
With rates of medical implant use only set to rise - along with their associated complications – this is one technology poised for large impact.