Introduction
Driving cessation for older adults with dementia and their family/friend carers is a complex, challenging, and emotion-laden process (Holden and Pusey, Reference Holden and Pusey2021; Sanford et al., Reference Sanford2019, Reference Sanford, Naglie, Cameron and Rapoport2020) that is considered one of the toughest issues in dementia care (McCracken et al., Reference McCracken, Caprio-Triscott and Dobbs2001). At stake in the decision to stop driving is the person’s independence, identity, social connectedness, and quality of life counterbalanced with their own and others’ safety (Carr and O’Neill, Reference Carr and O’Neill2015; Perkinson et al., Reference Perkinson2005). Driving cessation in older adulthood is associated with many adverse health and psychosocial consequences (e.g. depression, anxiety, increased risk of institutionalization) (Chihuri et al., Reference Chihuri2016) that are further amplified for people with dementia. The decision to stop driving is complicated by the absence of reliable and valid office-based fitness to drive screening measures (Molnar et al., Reference Molnar, Patel, Marshall, Man-Son-Hing and Wilson2006) along with adequate training and education available for healthcare professionals on this topic (Sinnott et al., Reference Sinnott, Foley, Forsyth, McLoughlin, Horgan and Bradley2018). In addition, there is lack of understanding about dementia’s impact on driving ability (Liddle et al., Reference Liddle, Bennett, Allen, Lie, Standen and Pachana2013), lack of insight about one’s own declining abilities (Scott et al., Reference Scott, Liddle, Pachana, Beattie and Mitchell2020b), family carers’ and primary care physicians’ avoidance of difficult conversations about driving (Adler and Kuskowski, Reference Adler and Kuskowski2003; Byszewski et al., Reference Byszewski, Molnar and Aminzadeh2010), limited access to alternative transportation (Holden and Pusey, Reference Holden and Pusey2021; Sanford et al., Reference Sanford, Naglie, Cameron and Rapoport2020), and intense emotional ramifications (Sanford et al., Reference Sanford2019).
In addition to these challenges, more than three decades of research on driving cessation and dementia have highlighted recommendations and strategies aimed at supporting ongoing mobility and health. Nevertheless, gaps in meeting the needs of people with dementia and their family carers continue to prevail (Sanford et al., Reference Sanford, Naglie, Cameron and Rapoport2020; Stasiulis et al., Reference Stasiulis, Rapoport, Sivajohan and Naglie2020). Such a deficiency in the available research knowledge and its application in practice is known in the knowledge translation field as the “knowledge-to-action (KTA) gap” (Graham et al., Reference Graham2006). We aimed to address this gap at the individual and family levels through the development of an intervention framework and a driving cessation toolkit directed to people with dementia and their family/friend carers.
People with dementia and their family members are largely ill-equipped to manage the challenges and ethical dilemmas surrounding the decision to stop driving (LaFrance et al., Reference Lafrance, Dreise, Gouliquer and Poulin2021). However, with the administration of timely education and resources, the risk of unsafe driving and injury, as well as the potential trauma and the negative effects of this major life transition, can be lessened (Sanford et al., Reference Sanford, Naglie, Cameron and Rapoport2020). Studies indicate that early discussions about driving and about dementia’s progressive impact on driving abilities can increase the likelihood of shared decision-making by people with dementia (Byszewski et al., Reference Byszewski, Molnar and Aminzadeh2010; Scott et al., Reference Scott, Liddle, Pachana, Beattie and Mitchell2020b). Planning for, and providing practical support to help people maintain their participation in social and daily activities, is considered integral to lessening the grief and anger associated with the loss of independence and identity (Holden and Pusey, Reference Holden and Pusey2021; Sanford et al., Reference Sanford2019). Equipping family carers with knowledge and resources is important as they are often depended on to observe and assess the person with dementia’s driving abilities (Adler et al., Reference Adler, Rottunda, Rasmussen and Kuskowski2000) and play a key role in decision-making about driving (Adler, Reference Adler2010; D’Ambrosio et al., Reference D’Ambrosio, Coughlin, Mohyde, Carruth, Hunter and Stern2009). In addition, family members report feeling ill-equipped yet responsible for navigating the licensing and reporting system (Chacko et al., Reference Chacko, Wright, Worall, Adamson and Cheung2015; Liddle et al., Reference Liddle, Tan, Liang, Bennett, Allen, Lie and Pachana2016). Supportive strategies and resources to help family carers manage the emotional impact of driving cessation, including feelings of resentment, frustration, burden, and guilt are scarce (Chacko et al., Reference Chacko, Wright, Worall, Adamson and Cheung2015; Sanford et al., Reference Sanford, Naglie, Cameron and Rapoport2020).
Despite the rapidly increasing number of drivers with dementia and the need for resources, few evidence-based interventions exist (Rapoport et al., Reference Rapoport, Cameron, Sanford and Naglie2017; Sinnott et al., Reference Sinnott, Foley, Horgan, McLoughlin, Sheehan and Bradley2019). Literature describing the development and/or evaluation of other interventions and resources include manual-based toolkits (Byszewski et al., Reference Byszewski2013; Jouk and Tuokko, Reference Jouk and Tuokko2017), a decision aid targeted to people with dementia (Carmody et al., Reference Carmody, Potter, Lewis, Bhargava, Traynor and Iverson2014; Chang et al., Reference Chang2021) and more recently a health-care provider delivered driving cessation program for drivers with dementia that includes a module for family carers (Scott et al., Reference Scott, Liddle, Mitchell, Beattie and Pachana2019, Reference Scott2020a, Reference Scott, Liddle, Pachana, Beattie and Mitchell2020b). Positive outcomes have been found for some of these interventions including lower rates of depressive symptoms, increased likelihood to discuss driving cessation, increased number of trips out of home after driving cessation (Rapoport et al., Reference Rapoport, Cameron, Sanford and Naglie2017), and improved knowledge that helped with decision-making among people with dementia (Carmody et al., Reference Carmody, Potter, Lewis, Bhargava, Traynor and Iverson2014; Chang et al., Reference Chang2021).
Despite the potential availability of these, albeit limited, interventions, and other resources, people with dementia and family/friend carers report a lack of support and information (Croston and Meuser, Reference Croston and Meuser2009; Liddle et al., Reference Liddle, Bennett, Allen, Lie, Standen and Pachana2013). During our own research activities to develop a multi-faceted educational resource, we identified a gap in the access (i.e. easily retrievable), usability (i.e. content, language, and design that is appropriate for people with dementia), trustworthiness (i.e. confidence that the information is valid and based on evidence), and knowledge (i.e. awareness) about existing resources and tools to support people with dementia and their family carers. (Rapoport et al., Reference Rapoport2019; Sanford et al., Reference Sanford2016).
To bridge the divide between what is known about driving cessation and dementia (i.e. challenges and strategies to support driving cessation) and what is actually used in the real world (tools and resources), we produced an intervention framework that identified key gaps in which knowledge users require information and support. These gaps informed the development of a toolkit, called the Driving and Dementia Roadmap (DDR). Barac and colleagues (2014, p.2) define toolkits as “the bundling of a combination of educational materials… presented in a variety of formats used to inform and improve health behaviors for diverse audiences, including health practitioners, patients, community and health organizations, policy makers and for the public.” As a knowledge translation strategy in healthcare, toolkits are considered an effective approach for facilitating evidence use in practice and improving health outcomes (Barac et al., Reference Barac, Stein, Bruce and Barwick2014; Yamada et al., Reference Yamada, Shorkey, Barwick, Widger and Stevens2015). This paper reports on our process of using a KTA approach in developing a web-based resource/toolkit to support people with dementia and their family/friend carers in the decision-making process and transition to non-driving. We summarize the myriad of research activities comprising the knowledge creation and action cycle phases that resulted in the DDR. Notably, our detailed reporting of the knowledge creation phase is an area in knowledge translation research not well documented in previous studies employing the KTA framework (Field et al., Reference Field, Booth, Ilott and Gerrish2014). This paper builds on earlier publications about driving cessation and dementia in International Psychogeriatrics by addressing the identified challenges that people with dementia and family/friend carers face in the decision-making and transition to non-driving (Liddle et al., Reference Liddle, Tan, Liang, Bennett, Allen, Lie and Pachana2016, Reference Liddle, Bennett, Allen, Lie, Standen and Pachana2013) that healthcare providers are often not equipped to deal with (Scott et al., Reference Scott2020a, Reference Scott, Liddle, Pachana, Beattie and Mitchell2020b; O’Neill, Reference O’Neill2020; Cameron et al., Reference Cameron2017). It also takes up the call for needed research on knowledge translation/implementation science in the psychogeriatric field (Pachana, Reference Pachana2020, Reference Pachana2021; Parker and Syme, Reference Parker and Syme2021).
Methods
KTA framework
We chose the well-established KTA knowledge translation conceptual framework (Graham et al., Reference Graham2006) because it provides a practical and flexible approach, geared to applying research findings and leading to the development of knowledge tools or products – a primary objective of our knowledge translation plan. It also ensures the involvement of knowledge users, which aligns with our commitment to person-centered care (Graham et al., Reference Graham2006). The KTA attends to the ways in which knowledge is created, adapted, and evaluated in local contexts. The framework is comprised of two separate but interrelated parts: 1) knowledge creation and 2) action cycle. Knowledge creation is conceptualized as a funnel involving three phases of knowledge distillation including “knowledge inquiry” (i.e. primary studies); “synthesis” (i.e. systematic reviews, scoping reviews, and meta-analyses); and the resulting “knowledge product” (e.g. decision aids, frameworks, and toolkits). This final phase reflects the most refined knowledge that is tailored in user-friendly fashion to end-users based on their informational needs, thus facilitating the KTA goal of knowledge uptake and application (Graham et al., Reference Graham2006).
Through a series of seven phases, the action cycle outlines the process of activities required for effective knowledge application. In practice, the phases are not necessarily sequential, with movement between the phases and the cycles occurring in an iterative and dynamic manner. Critical to this overall process is the involvement of knowledge users (e.g. people with dementia, family/friend carers, healthcare and service providers) who can help to ensure the applicability of the knowledge products (Straus et al., Reference Straus, Tetroe and Graham2009).
Our work within the KTA Framework is depicted in Figure 1. In this paper, we report mainly on the knowledge creation process, and the intersection with two of the action cycle phases (adapting knowledge to local contexts and assessing barriers to knowledge use) that pertains to the work conducted thus far. In our application of the KTA framework, we have slightly modified the knowledge creation phases by incorporating two funnels of knowledge distillation: One leading to the creation of our intervention framework, the “Driving and Dementia Intervention Framework (DD-IF)” and the second to the production of our toolkit, the “DDR,” which is directly informed by the DD-IF.
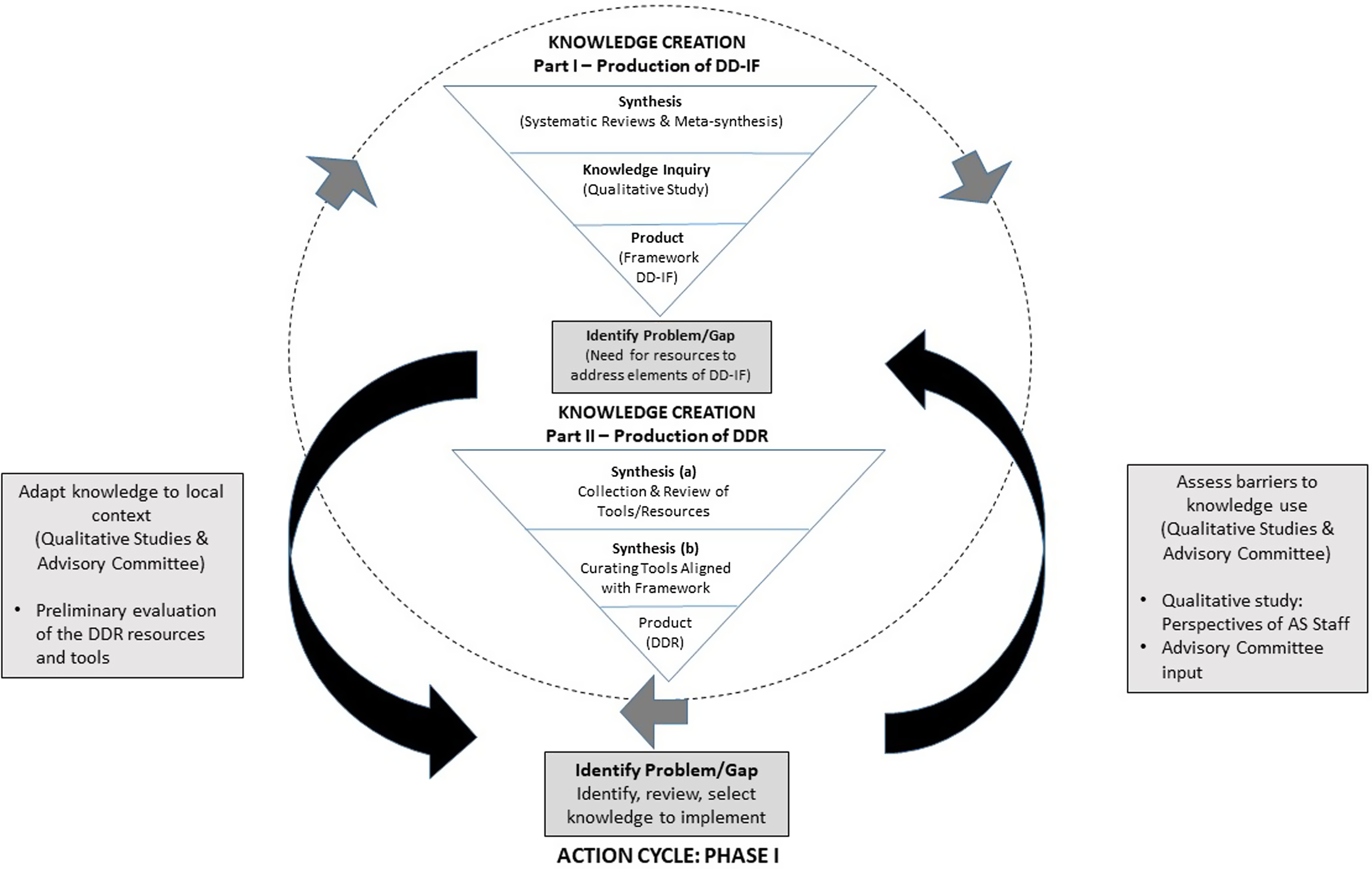
Figure 1. Adapted KTA Framework.
Knowledge creation part I: production of the DD-IF
The first funnel of our knowledge creation activities resulted in the production of the DD-IF. Our overall purpose in Part I was to distill knowledge that would inform the content and design of a supportive driving cessation intervention for people with dementia and their family/friend carers. More details about the studies, including analyses that were conducted that led to the findings, can be found in the associated referenced papers.
Synthesis: systematic review and meta-synthesis
As part of the “synthesis phase,” we conducted a systematic review on driving cessation interventions in individuals with dementia and older adults (Rapoport et al., Reference Rapoport, Cameron, Sanford and Naglie2017) as well as on interventions targeting other major life transitions in later life (Vrkljan et al., Reference Vrkljan, Montpetit, Naglie, Rapoport and Mazer2019). Systematic reviews were chosen to gain an overview of interventions in the literature and to identify effective strategies that could be considered in supporting driving cessation. To obtain a deeper understanding of the factors that influence the experiences of driving cessation in the context of dementia and thus inform the development of effective programs to support individuals through this process, a meta-syntheses of qualitative studies on dementia and driving were also conducted (Sanford et al., Reference Sanford, Naglie, Cameron and Rapoport2020). The synthesis of knowledge via systematic reviews and meta-syntheses is considered foundational to knowledge translation (Straus et al., Reference Straus, Tetroe and Graham2009).
Knowledge inquiry: qualitative study
The “knowledge inquiry” phase involved a qualitative study exploring key stakeholders’ perspectives on the process and strategies that facilitate decision-making, coping, and adapting to driving cessation (Sanford et al., Reference Sanford2019). Qualitative methods were chosen to facilitate an in-depth exploration of affected individuals’ emotional experiences, viewpoints, and needs in order to further understanding about the driving cessation process. Three focus groups were conducted with 10 family carers and in-depth interviews took place with 10 healthcare providers, six organizational representatives, two former drivers with dementia, and three family members. Analytic themes were generated through an iterative and inductive process of standard thematic analysis (Braun and Clarke, Reference Braun and Clarke2006) (Supplementary Table).
Product: DD-IF
Based on evidence from the knowledge inquiry (i.e. qualitative study on key stakeholders’ perspectives) and synthesis phases (i.e. systematic reviews and meta-synthesis), we identified elements to include in a driving cessation intervention. The Trans-theoretical Model (TM) of behavior change (Prochaska and Velicer, Reference Prochaska and Velicer1997) was employed to inform and guide the content of these elements and their organization across a continuum of driving cessation decision-making and adapting stages. The TM posits that driving behavior change is impacted by the actions of each successive stage. For example, planning for alternative ways to remain mobile in the contemplative stage directs behavior in the decision to stop driving and adaptation to post-driving (Sanford et al., Reference Sanford, Naglie, Cameron and Rapoport2020). The resulting DD-IF (Figure 2) encompasses the practical and emotional elements that characterize the driving cessation process and formed the foundation on which the DDR was built.
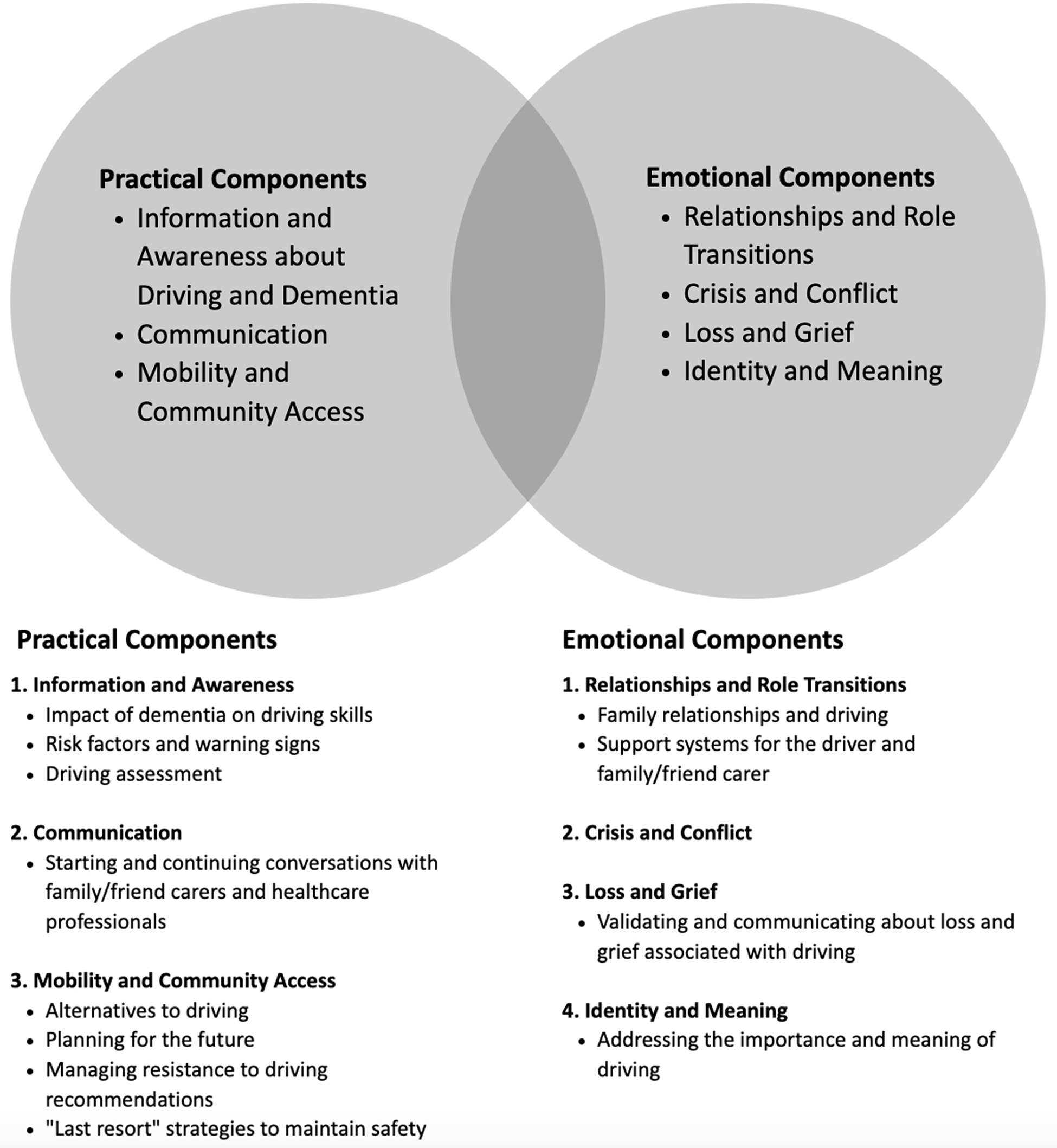
Figure 2. Driving and Dementia Intervention Framework.
Knowledge creation part II: production of the DDR
Our second knowledge creation funnel, comprised of further knowledge synthesis activities, culminated in the production of an early version of the DDR. Through the processes detailed below, knowledge about driving cessation was distilled into a usable format for people with dementia and family/friend carers.
Synthesis II(a): collection and review of resources and tools (Figure 3)
In the first phase, relevant resources and tools were collected via informal consultations with other stakeholders (e.g. clinician researchers, healthcare providers), reviewing publications of relevant tools, as well as Internet and website searches. For our purposes, a “resource” contains more than one tool or segments of text that can be extracted and applied to elements of the DD-IF. Internet Google and relevant website (e.g. Alzheimer Society) searches involved using key terms such as “driving cessation” and “tools” or “resources.” Three co-investigators (MR, GN, SS) reviewed the list of 40 resources and 13 tools that were identified and selected those for further review by the wider investigative team based on whether they addressed driving or driving cessation; were created for people with dementia and/or family/friend carers; were applicable to multiple geographic areas; and were up-to-date.

Figure 3. Knowledge Creation Part II.
In the second phase, the selected 12 resources and 7 tools were then reviewed and their suitability was determined by four researcher pairs. Areas of assessment included content, accessibility, published evidence, relevance to driving cessation and people with dementia, and to the target groups (i.e. drivers and former drivers with dementia, family/friend carers, healthcare/service providers). Each reviewer’s dyad reached a consensus based on the assessment variable. Discussions to resolve conflicts and finalize the assessments were held between reviewer pairs and a third-party researcher who had previously reviewed the resources/tools. Two resources were excluded and a total of 10 resources and seven tools, which included guidebooks, videos, driving assessments, and information sheets were selected.
Synthesis II(b): resources and tools curated and aligned with DD-IF
The next step of the knowledge distillation and refinement process involved curating the resources and tools identified and selected in synthesis II(a) (Figure 1) to align with the elements (e.g. communication, mobility, and community access) of the DD-IF. From the ten selected resources, 64 distinct tools (e.g. worksheets, sections of text) were extracted to be reviewed. A refined review of the 64 tools and the remaining 7 tools plus four new tools identified by the research team, for a total of 75 tools, was conducted independently by three researchers (ES, GN, MR) who then met to discuss their assessments (e.g. format, style, readability, alignment with the DD-IF elements, uniqueness). A consensus to select 32 tools and 5 additional newly identified tools was achieved. These were later pared down to 24 tools to minimize replication of content (Table 1). Written permission was obtained to include the tools in the DDR.
Table 1. Tools in driving and dementia roadmap

Product: early version of the DDR
Concurrent with the knowledge creation activities in synthesis II(a), we developed an early PowerPoint demonstration version of the DDR – a collection of selected tools to be aligned with the DD-IF elements. The initial iteration of the DDR, prior to the final selection of 24 tools (synthesis activities II(b)), took the form of a website created by our research team using Google Sites, a no-cost website building platform. The purpose of this site was to familiarize users (stakeholder study participants) with the elements of the DD-IF and the initially selected resources, and tools, which were categorized as guidebooks (resources containing distinct tools such as worksheets), driving assessments, videos, and advanced driving directives. Our intent was to use this version of the DDR in the action cycle of the KTA for its further development and refinement once the final list of resources and tools was refined.
Action cycle: adapting and refining to implement the DDR
In tandem with the knowledge creation phases, we engaged with phases of the action cycle to ensure the evolving DDR’s accessibility and relevance to people with dementia and family/friend carers. This was an iterative and dynamic process, as characteristic of the KTA framework, which included reviewing and selecting knowledge (e.g. DDR content, resources and tools), adapting knowledge to local contexts (value, usefulness, and appropriateness of the DDR), and assessing the determinants of knowledge use (barriers and facilitators) (Graham et al., Reference Graham2006; Straus et al., Reference Straus, Tetroe and Graham2009). The research activities, as described below, informed the ongoing development and refinement of the DDR, including its content, design, and format. Drawing from end-users’ experiences to tailor the DDR and adapt it to local contexts was a key objective in this phase.
Preliminary evaluation of the DDR resources and tools
Prior to the Google Sites iteration of the DDR, a preliminary evaluation of the DDR resources and tools and their alignment with the DD-IF as presented in PowerPoint by the principal investigators (GN and MJR) was conducted. The objective was to collect preliminary data on key informants’ perspectives about the DDR and to inform subsequent data collection processes for the purpose of facilitating the DDR’s effective implementation in community-based settings (e.g. AS organizations) (Naglie et al., Reference Naglie, Sanford and Rapoport2018). A focus group was held in collaboration with an AS organization in Ontario following the presentation. The focus group (n = 8) was comprised of six family members of drivers or former drivers with dementia, one former driver with dementia, and a social worker. Participants were asked about their impressions of the DD-IF and the DDR. Data were analyzed using inductive thematic coding (Braun and Clarke, Reference Braun and Clarke2006) (Supplementary Table). The main themes that emerged included recommendations to consider the DDR users’ age, family context, and stage of driving cessation as well as ensuring that the DDR promoted a sense of autonomy. These findings informed the organization of the DDR to include separate portals targeting people with dementia and family/friend carers of people with dementia who were still driving and who had stopped driving.
Qualitative study: perspectives of AS staff
As a precursor to our implementation evaluation of the DDR in Canadian AS organizations, we conducted a qualitative study exploring the perspectives of 15 AS staff on the Google Sites web-based version of the DDR (Stasiulis et al., Reference Stasiulis, Rapoport, Sivajohan and Naglie2020). In addition to obtaining feedback on the DDR, our objective was to inform strategies that would support implementation in these settings. Overall, the DDR was favorably viewed as addressing a gap in accessible and trusted resources on driving cessation for people with dementia and their family/friend carers. Resulting recommendations included ensuring that materials directed to people with dementia are understandable (i.e. appropriate design and language); incorporating resources that address the emotional impact of driving cessation, strategies to encourage discussions about driving as well as information on region-specific licensing regulations (Supplementary Table).
Building the DDR: engaging with the advisory group
The building of the final web-based DDR involved a team of web developers, a graphic designer, and a plain language content writer. Over a period of ten months, after refining the pilot DDR based on study participants’ feedback described above, we engaged in an ongoing iterative fashion with an Advisory Group to obtain detailed feedback on the DDR’s content as well as on its format and design. The Advisory Group was comprised of four people living with dementia and four family carers. The content and tools were described as “excellent.” While advisors liked the DDR’s overall format and design, they suggested increasing font sizes, collapsing topics into fewer categories to reduce the number of choices, using images with more diverse representation of people (e.g. various cultural backgrounds and ages), and employing positive person-centered language (i.e. avoiding negative terms such as “burden”).
Results
The product: web-based DDR
Built on a web-based platform, the DDR (www.drivinganddementia.ca) contains separate portals aimed at three specific audiences: people with dementia, family/friend carers, and healthcare providers (the latter was developed during manuscript preparation and is not described further in this manuscript) (see Figure 4 for a schematic outline of the DDR). Drawing from the findings of the qualitative studies and informed by the TM, each portal is divided into two sections targeting the person with dementia based on their driving status, as “still driving” or “no longer driving.” Within each, users are presented with sections on topics related to driving cessation derived from the DD-IF (Figure 2). Content in each section was formulated based on literature reviews, qualitative studies, available resources, as well as the clinical experiences of two of the authors who are physicians specialized in care for older adults (GN, MR). As shown in Table 1, 24 discrete tools consisting of worksheets, videos, driving assessments, and decision aids, which individually address different aspects of the driving cessation process, were incorporated into the DDR as they aligned with the audience type and stage of driving cessation. An additional resource will include a lay person’s synopses and links to the pertinent licensing and reporting regulations for medically unfit drivers in each Canadian province and territory. In summary, the DDR provides a one-stop, online comprehensive repository of expertly reviewed tools with guided access to specific content and unique portals for people with dementia, family/friend carers who are at varied stages in the driving cessation process.

Figure 4. Driving and Dementia Roadmap Outline.
Discussion
This paper contributes to the knowledge translation literature as well as to the driving cessation and dementia field by detailing a KTA process that resulted in a contextually relevant, accessible educational resource/toolkit, the DDR. To our knowledge, the DDR is the only online toolkit geared specifically to this audience that comprehensively addresses the fundamental aspects of decision-making and transitioning to non-driving. A critical component of the KTA framework (Graham et al., Reference Graham2006), which guided the DDR’s development, was the involvement of key stakeholders (drivers with dementia, family and friend carers, healthcare and service providers) who participated in a series of knowledge exchange activities that enhanced the relevance, usability, and accessibility of the DDR. Although the content areas of the DDR align closely with the seven-module CarFreeMe-People with Dementia intervention (Scott et al., Reference Scott2020a), CarFreeMe is an intervention delivered by a health professional, whereas the DDR can be accessed directly by people with dementia and family carers.
The flexibility and adaptability of the KTA model proved conducive to our progression in developing the DDR that entailed two funnels of knowledge distillation in the knowledge creation phase. From our research activities in the first funnel (i.e. systematic reviews, meta-analyses, qualitative study), we identified critical elements to address in the driving cessation process that were operationalized into the DD-IF. In addition to the gap in interventions supporting people with dementia and family carers, we identified an opportunity to improve the accessibility and usability of publicly available resources and tools. Hence, with the aim to build a scalable resource (i.e. toolkit) guided by the elements of the DD-IF, we continued our knowledge creation activities as depicted in the second funnel. The collection, review, distillation, and curation of resources and tools culminated in an early version of the DDR. Our adaption of the KTA framework to include two knowledge creation funnels attests to the KTA’s practicality and flexibility allowing for its application in idiosyncratic ways that were integral to our study (Field et al., Reference Field, Booth, Ilott and Gerrish2014). The detailed reporting of our knowledge creation phase also contributes to the knowledge translation field. According to a systematic review, most studies employing the KTA framework in an integrative way provided details only on the action cycle phase of their projects (Field et al., Reference Field, Booth, Ilott and Gerrish2014).
Research activities in the action cycle (review and curation of resources/tools, two qualitative studies and Advisory Group feedback) that followed our pilot version of the DDR resulted in substantial revisions to the DDR. These changes reflect the objective of the action cycle, which is to ensure that the application of knowledge results in actions that ultimately enhance health status (Graham et al., Reference Graham2006); in our case the health and wellness of people with dementia and their family/friend carers. For action to occur, the knowledge being translated must be relevant, appropriate, applicable, timely, and suit the needs of the end-users (Campbell, Reference Campbell2010). By following these three action cycle steps: 1) reviewing and selecting knowledge; 2) adapting knowledge to local contexts; 3) and assessing barriers and facilitators to knowledge use, we integrated changes to the pilot DDR’s content, design, and mode of delivery to facilitate implementation and uptake in community-based settings that support people with dementia.
Changes included extracting tools from identified resources (e.g. guidebooks) and writing content on topics related to the elements of the DD-IF, rather than solely integrating or directing users to third-party resources and tools. Other revisions derived from the action cycle activities were related to the DDR’s format, design, and language style. For example, to facilitate an individualized approach to driving cessation support, separate portals for people with dementia still driving or no longer driving were incorporated. To promote a sense of autonomy, edits to the content were made to reflect person-centered and dementia-friendly language. Other revisions to ensure the DDR’s usability for people with dementia included reduced text, less topic choices, and numbering headings. These adaptations are illustrative of the iterative and dynamic movement that can occur between the action cycle and knowledge creation components (Graham et al., Reference Graham2006). The action cycle processes also confirmed the relevance and applicability of the content areas such as awareness about dementia’s impact on driving, strategies to encourage discussions about driving, and addressing the emotional implications.
The factors that have contributed to the popularity of toolkits as a knowledge translation strategy in healthcare were also appealing considerations for choosing a toolkit format. Namely, toolkits offer flexible tool selection, tend to be practical and action-oriented (Barac et al., Reference Barac, Stein, Bruce and Barwick2014; Yamada et al., Reference Yamada, Shorkey, Barwick, Widger and Stevens2015), and are a relatively low-cost knowledge translation intervention (Salbach et al., Reference Salbach2021). Located on a virtual platform, toolkits, such as the DDR, are more easily accessible to a wider range of audiences (Barac et al., Reference Barac, Stein, Bruce and Barwick2014). In addition to implementing the DDR in organizations and clinical settings that support older adults with dementia (e.g. Alzheimer Society, memory clinics), we will employ dissemination strategies (e.g. social media) to reach people outside of these settings. This is consistent with feedback provided by our AS study participants, who noted the importance of resources that could be accessed by people who are not involved with such organizations (Stasiulis et al., Reference Stasiulis, Rapoport, Sivajohan and Naglie2020).
Our employment of the KTA framework aligns with research on the effectiveness of toolkits and the recommendation by implementation science to use theories, models, and frameworks as a base to build interventions such as toolkits (Damschroder, Reference Damschroder2020; Salbach et al., Reference Salbach2021; Yamada et al., Reference Yamada, Shorkey, Barwick, Widger and Stevens2015). Utilizing this framework meant that we were able to meet all the recommendations and suggestions for toolkit development recently produced by a panel of experts that included: usability testing (via feedback from potential users); exploring the needs of potential users early in the developmental phase; incorporating behavioral theory (i.e. we used the TM); and including pilot testing (Hempel et al., Reference Hempel2019). The resulting characteristics of the DDR include features identified as positively impacting the application of toolkits into practice such as specifying the targeted audiences; identifying the objectives of the resources and tools (Davis et al., Reference Davis, Howk, Spurlock, McGinnis, Cohen and Fagnan2017); and providing guidance on how to use the tools (Yamada et al., Reference Yamada, Shorkey, Barwick, Widger and Stevens2015).
These quality characteristics of toolkits, however, do not always ensure effective implementation of the toolkit in practice (Yamada et al., Reference Yamada, Shorkey, Barwick, Widger and Stevens2015). Contextual factors, such as organizational needs and structures, local barriers, and practice facilitation support (i.e. engagement skills), can impact uptake of the DDR (Davis et al., Reference Davis, Howk, Spurlock, McGinnis, Cohen and Fagnan2017). Research detailing the implementation process and outcomes of toolkits is very limited (Hempel et al., Reference Hempel2019; Yamada et al., Reference Yamada, Shorkey, Barwick, Widger and Stevens2015). Currently, our team is analyzing the results of an implementation evaluation of the DDR we conducted in AS organizations across Canada. To guide the evaluation, we followed the latter phases of the KTA framework (e.g. select, tailor and implement interventions and monitor knowledge use) (Graham et al., Reference Graham2006).
A limitation of the field, which impacted the DDR’s development was the lack of published evidence supporting the tools being considered for inclusion in the DDR. This meant that the evaluation process tended to be based on the subjective views of the reviewer dyads about acceptability, adaptability, and effectiveness. Nevertheless, our team of clinician reviewers with expertise in older adult care and driving and dementia conducted a rigorous process to identify and review publicly available resources, and tools. This collaborative process of independent and collective reviews as well as feedback from AS frontline staff and our Advisory Group contributed to the trustworthiness of the selected tools. Another field limitation was the dearth of available tools that addressed the emotional implications of driving cessation. To address this gap, we drew from the limited available resources to develop content about the emotions that family/friend carers and people with dementia may experience when they stop driving as well as strategies to help them manage these feelings.
As a web-based resource, the DDR may pose limitations to individuals who do not have adequate access to the internet or are not comfortable using technology, particularly as dementia progresses. However, preliminary findings from our implementation evaluation of the DDR in AS settings indicated that AS staff and family/friend carers were able to facilitate people with dementia’s effective use of the DDR by going through it with them (unpublished).
Conclusion
Driving cessation is a major life transition that not only affects drivers with dementia but also their family/friend carers and health professionals (Holden and Pusey, Reference Holden and Pusey2021). In developing the DDR, our aim was to address the complex challenges and ramifications that driving cessation poses for individuals during this transition process. Guided by the KTA framework, we engaged in a systematic and iterative process of knowledge creation and translation, resulting in a person-centered, individualized, accessible, and flexible resource. As detailed in this paper, the KTA process was integral to the DDR’s development. Amidst the limited accessibility of knowledge, tools, and resources, the DDR is a much-needed support that can help people with dementia and their families maintain their mobility, community participation as well as social and emotional wellbeing.
Conflict of interest
None.
Source of funding
This project is part of the Canadian Consortium on Neurodegeneration in Aging (CCNA; Grant number 201312CNA-322265-CNA-CFAF-32054). The CCNA is supported by a grant from the Canadian Institute of Health Research with funding from several partners. Funding for this project was also provided by the AHSC AFP Innovation Fund and the Centre for Aging and Brain Health Innovation. Funding for this project was also provided by the Centre for Aging and Brain Health Innovation and the Ontario AHSC AFP Innovation Fund.
Description of authors’ roles
E. Stasiulis and S. Sanford managed the project at separate periods and were involved in all aspects of study design, implementation, and analysis as well as reviewing and curating tools and resources. E. Stasiulis prepared the first draft of the manuscript. S. Sanford contributed to all drafts of the manuscript. G. Naglie and M. Rapoport were co-principal investigators of the project, supervised all aspects of study design and implementation including reviewing and curating the resources and tools as well as contributing to the writing of the paper. P. Moorhouse provided input into study design, reviewed resources and tools for inclusion in the DDR, and reviewed the final manuscript. A. Crizzle was involved in data collection contributing to the DDR and in reviewing the draft manuscript. M. Porter was involved in reviewing resources and tools as well as the draft manuscript. B. Vrkljan and B. Mazer co-led the review of transitions in older adults and edited the final manuscript. B. Mazer also reviewed the resources and tools. A. Myers was involved in the grant proposal and reviewing the manuscript. P. Belchior reviewed the resources and tools for inclusion in the DDR and reviewed the final transcript. I. Gélinas contributed to the conceptualization and design of the project and reviewed the manuscript.
Acknowledgements
We would like to thank Vivian Nash and Steve Mahfouda of Blue Lemon Media for the web design of the DDR; Naomi Shacter for creating the DDR logo; and Carolyn Wilby for ensuring the DDR’s content was clearly written and appropriate for the targeted audiences. We are also thankful for Harvir Sandhu’s preparation of the driving license and reporting regulations for each of the provinces and territories in Canada. Finally, we are grateful to Michel Bédard for his contributions to the project.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/S1041610222001235









