Up until recently, if bacteria were detected in your blood you would be in a world of trouble. Blood was long considered to be sterile, meaning free of viable microorganisms like bacteria. When disease-causing bacteria spread to the blood, they can cause a life-threatening septic shock.
But the use of DNA sequencing technology has allowed researchers to more easily detect something that had been reported as early as the late 1960s: bacteria can be found in the blood and not cause disease.
As we begin to map out and understand the complex microbial ecosystem that lives in our gut and elsewhere in the body, we contemplate an important question: is there such a thing as a blood microbiome?
Detecting a fingerprint in the blood
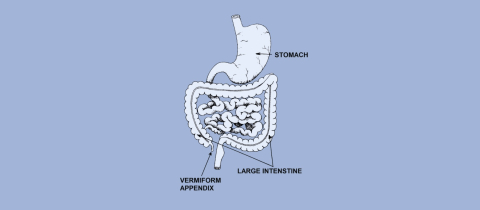
Our large intestine is not sterile; it is teeming with bacteria. But there are parts of the body that were long thought to be devoid of microorganisms. The brain. Bones. A variety of internal fluids, like our synovial fluid and peritoneal fluid. And, importantly, the blood.
Blood is made up of a liquid called plasma filled with red blood cells, whose main function is to carry oxygen to our cells. It also transports white blood cells, important to monitor for and fight off infections, as well as platelets, involved in clotting.
In the 1960s, a team of Italian researchers published multiple papers describing “mycoplasm-like forms”—meaning shapes that look like a particular type of bacteria that often contaminate cells cultured in the lab—in the blood of healthy people. This finding was confirmed in 1977 by a different team, which reported that four out of the 60 blood samples they had drawn from healthy volunteers showed bacteria growing in them. These types of tests, however, were rudimentary compared to what we have access to now. In the 2000s, they were mostly supplanted by DNA testing.
While we can sequence the entire DNA of any bacteria found in the blood, the technique most often used is 16S rRNA gene sequencing. I have always admired physicists’ penchant for quirky names: gluons, neutrinos, and charm quarks. Molecular biologists, by comparison, tend to be more sober. Yes, we have genes like Sonic hedgehog and proteins called scramblases; usually, though, we have to contend with the dryness of “16S rRNA.” You see, RNA is a molecule with many uses. Messenger RNA (or mRNA) acts as a disposable copy of a gene, a template for the production of a specific protein. Transfer RNA (or tRNA) actually brings the building blocks of a protein to where they are being assembled. And ribosomal RNA (or rRNA) is the main component of the giant protein factories in our cells known as ribosomes. One of its subunits is made up of, among others, a particular string of RNA known as the 16S rRNA.
The cool thing about the gene that codes for this 16S rRNA molecule is that it is very old and it mutates at a slow rate. By reading its precise sequence, scientists can tell which species it belongs to. Most of the studies of the putative blood microbiome use this technique to tell which species of bacteria are present in the blood being tested. The limitation of this test, however, is that dead bacteria have DNA too. The fact that DNA from the 16S rRNA gene of a precise bacterial species was detected in someone’s blood does not mean these bacteria were alive. For there to be a microbiome in the blood, these microorganisms need to live.
Which brings us to another important point of discussion. In order for scientists to agree that a blood microbiome exists, they first need to decide on the definition of a microbiome, and this is still a point of contention. In 2020, while companies were more than happy to sell hyped-up services testing your gut microbiome and claiming to interpret what it meant for your health, actual experts in the field met to agree on just what the word meant. “We are lacking,” they wrote, “a clear commonly agreed definition of the term ‘microbiome’.” For example, do viruses qualify? A microbiome implies life but viruses live on the edge, pun intended: they have the genetic blueprint for life yet they cannot reproduce on their own.
These experts proposed that the word “microbiome” should refer to the sum of two things: the microbiota, meaning the living microorganisms themselves, and their theatre of activity. It’s like saying that the Earth is not simply the life forms it houses, but also all of their individual components, and the traces they leave behind, and the environmental conditions in which they thrive or die. The microbiome is made up of bacteria and other microorganisms, yes, but also their proteins, lipids, sugars, and DNA and RNA molecules, as well as the signalling molecules and toxins that get exchanged within their theatre. (This is where viruses were sorted, by the way: not as part of the living microbiota but as belonging to the theatre of activity of the microbiome.)
The microbiome is a community, and this community has a distinct habitat.
So, what does the evidence say? Is our blood truly host to a thriving community of microorganisms or is something else going on?
Transient and sporadic
Initial studies of the alleged blood microbiome were small. The amounts of bacteria that were being reported based on DNA sequencing were tiny. If this microbiome existed, it seemed sparse, more “asteroid field in real life” than “asteroid field in the movies.”
An issue looming over this early research is that of contamination. If bacteria are detected in a blood sample, were they really in the blood… or did they contaminate supplies along the way? When blood is drawn, the skin, which has its own microbiome, is punctured. The area is usually swabbed with alcohol to kill bacteria, and the supplies used should be sterile, but suffice to say that from the blood draw to the DNA extraction to the DNA amplification to the sequencing of this DNA, bacteria can be introduced into the system. In fact, it is such common knowledge that certain bacteria are found inside of the laboratory kits used by scientists that this ecosystem has its own name: the kitome. One way to rule out these contaminants is to simultaneously run negative controls alongside samples every step of the way, to make sure that these negative controls are indeed free of bacteria. But early papers rarely reported when controls were used.
Last year, results from what purports to be the largest study ever into the question of whether the blood microbiome exists were published in Nature Microbiology. A total of 9,770 healthy individuals were tested. The conclusion? Yes, some bacteria could be found in their blood, but the evidence contradicted the claim of an ecosystem. In 84% of the samples tested, no bacteria were detected. In most of the other samples, only one species was found. In an ecosystem, you would expect to see species appearing together repeatedly, but this was not the case here. And the species they found most often in their samples were known to contaminate these types of laboratory experiments.
So, what were the few bacteria found in the blood and not recognized as contaminants doing there in the first place if they were not part of a healthy microbiome? The authors lean toward an alternative explanation that had been floated for many years: these bacteria are transient. They end up in the blood from other parts of the body, either because of some minor leak or through their active transportation into the blood by agents such as dendritic cells. Like pedestrians wandering off onto the highway, these bacteria do not normally live in the blood but they can be seen there when we look at the right moment.
Putting the diagnostic cart before the horse
This blood microbiome story could end here and simply be an interesting example of scientific research homing in on a curious finding, testing a hypothesis, and ultimately refuting it (or at the very least providing strong evidence against it). But given the incentives of modern research and the social-media spotlight cast on the academic literature, there are two slightly worrying angles here that merit discussion.
Scientists are more and more incentivized to find practical applications for their research. It’s not enough, for example, to study bacteria that survive at incredibly high temperatures; we must be assured that the DNA replication enzyme these bacteria possess will one day be used in laboratories all over the world to conduct research, identify criminals, and test samples for the presence of a pandemic-causing coronavirus.
In researching this topic, I came across many papers claiming the existence of “blood microbiome signatures” for certain diseases that are not known to be infectious. We are thus not talking about infections leaking in the blood and causing sepsis. I saw reports of signatures for cardiovascular disease, liver disease, heart attacks, even for gastrointestinal disease in dogs. The idea is that these signatures could soon be turned into (profitable) diagnostic tests. The problem, of course, is that these studies are based on the hypothesis that a blood microbiome is real; that its equilibrium can be affected by disease; and that these changes can be reliably detected and interpreted.
But if the blood microbiome is imaginary, we are just chasing ghosts. This is not unlike the time that scientists were publishing signatures of microRNAs in the blood for every possible cancer. When I looked at the published literature in grad school, I realized that the multiple signatures reported for a single cancer barely overlapped. They were just chance findings. Compare enough variables in a small sample set and you will find what appears to be an association.
My second concern is that the transitory leakage of bacteria into the blood, as evidenced by the recent Nature Microbiology paper, will be used as confirmation of a pseudoscientific entity: leaky gut syndrome. At the end of their paper, the researchers hypothesize that these bacteria end up in the blood because the integrity of certain barriers in the body are compromised during disease or during periods of stress. The “net” in our gut gets a bit porous, and some of our colon’s bacteria end up in circulation, though they are not causing disease as far as we can tell. A form of leaky gut is known to exist in certain intestinal diseases, likely to be a consequence and not a cause. But leaky gut syndrome, favoured by non-evidence-based practitioners, does not appear to be real, yet many websites portray it as the one true cause of all diseases, a real epidemic. Nuanced scientific findings have a history of being stolen, distorted, and toyed with by fake doctors to give credence to their pet theories. Though I have yet to see examples of it, I suspect work done on this hypothesized blood microbiome will similarly get weaponized.
You have been warned.
Take-home message:
- Our blood was long considered to be sterile, meaning free of viable microbes, unless a dangerous infection leaked into it, causing sepsis
- Studies have provided evidence for the presence of bacteria in the blood of some healthy humans, leading to the hypothesis that, much like in our gut, our blood is host to a microbiome
- The largest study ever done on the topic provided strong evidence against this hypothesis. It seems that when non-disease-causing bacteria find themselves in our blood, it is temporary and occasional