What is evidence-based practice?
Evidence-based practice (EBP) aims to maximize the effectiveness of psychological interventions through adherence to principles informed by empirical findings, clinical expertise, and client characteristics. The Canadian Psychological Association (CPA) Task Force on Evidence-Based Practice of Psychological Treatments (2012) defines EBP as follows:
Evidence-based practice involves the conscientious, explicit and judicious use of the best available research evidence to inform each stage of clinical decision-making and service delivery. This requires that psychologists apply their knowledge of the best available research in the context of specific client characteristics, cultural backgrounds, and treatment preferences.
- CPA Task Force on Evidence-Based Practice, 2012 (click here to download full report)
More specifically, evidence-based practice entails:
- Efforts to provide the best possible services (which minimize the risk of harm and maximize the chance of benefit) for those seeking psychological treatment.
- A reliance on peer-reviewed, scientific research evidence as the basis for treatment selection, with preferential attention given to studies based on research methodologies that control threats to both the internal and the external validity of the research findings.
- Respect for the dignity, lived experiences, and preferences of individuals seeking psychological treatment, as manifested by consistent communication and collaboration between the clinician and the service user.
- The monitoring and evaluation of services provided to clients and patients. Practitioners should regularly and systematically monitor clients’ reactions as well as changes in their symptoms and functioning throughout treatment. This can be done through progress tracking and outcome monitoring.
- A willingness on the behalf of practitioners to alter the treatment plan based on ongoing treatment monitoring, discussions with the client or patient, and a reconsideration of the relevant research evidence.
WATCH: What is evidence-based practice and why does it matter? BY: Dr. David. J. A. Dozois
In the context of evidence-based practice, the best available research evidence is drawn from treatment outcome, treatment process, and standard psychological research.
Evidence based practice relies on various sources and levels of evidence, the strength and relevance of which should be considered according to the hierarchy depicted below:
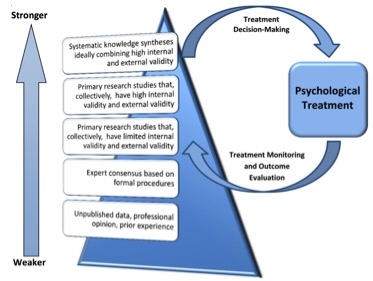
The best available evidence is highest on the hierarchy and includes findings that are replicated across studies and that used methodologies that are robust (i.e. that control threats to internal and external validity). Evidence stemming solely from unpublished professional opinion or prior clinical experience falls lower on the hierarchy, and should only be considered in the absence of relevant treatment research or high quality formal practice guidelines.
What is evidence-based practice and what is it not?
WATCH: What is evidence-based practice and what is it not? BY: Dr. Martin Drapeau
EBP is not the same as ESTs (empirically supported treatments):
- ESTs refer to specific psychological treatments that have been proven to be effective in controlled research for specific conditions. Whereas ESTs focus on specific therapeutic modalities and their use to treat specific problems or disorders, EBP is a broader approach to clinical decision-making which emphasizes the scientific evaluation of evidence along with patient or client preferences and characteristics. In other words, ESTs merely constitute a potential component of EBP.
EBP is not a “cookbook” approach to clinical practice:
- Clinicians using EBP do not simply “follow a recipe” – rather, they adopt an approach that integrates the best available scientific evidence with their clinical judgment and expertise to provide psychological treatment that is tailored to each client’s unique needs.
EBP does not involve equating a treatment with a diagnosis:
- EBP is not a “one-size-fits-all” approach to treatment. While a diagnosis may point a practitioner in the direction of a specific therapeutic intervention, most scientifically-informed interventions merely act as rough blueprints, affording practitioners significant leeway in terms of when and how to deliver treatment.
EBP does not rely solely on common factors in therapy:
-
Common factors theory proposes that different psychotherapeutic approaches in psychotherapy share common factors that account for a portion of the efficacy of a given treatment. EBP incorporates all evidence relevant to treatment outcomes, including common factors in psychotherapy, while bearing in mind specific client characteristics, cultural backgrounds, and individual treatment preferences.
Next: Benefits of EBP
Documents for download:
Content last reviewed: Sept, 2020


