
Enlarge
Donor: Dr. P Smyth
Date: 1921
Size (H x W x D cm): 14 x 13 x 9
Abbott No 49
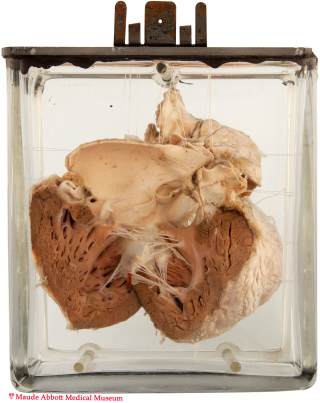
The pulmonary outflow tract and artery (A, long arrow) are markedly stenotic (lumen about 3 mm). The right ventricle free wall is thickened (5 mm). The aorta overlies a 1.8 cm ventricular septal defect (A, short arrows). A posterior view (B) shows blue rods in a small atrial septal defect.
A. Click image to enlarge. B. Click on image to enlarge.
History: Ten year-old boy with cyanosis and left hemiplegia.
Comment: The primitive heart consists of a straight tube whose proximal and distal ends are fixed within the pericardial cavity. Because the tube's growth is more rapid than that of the cavity, it is forced to bend, forming sulci and “segments” corresponding to future cardiac structures. The ascending limb of this bent structure (the bulbis cordis) differentiates into three components:
- proximal - the trabeculated portion of the right ventricle
- middle (the conus cordis) - the outflow tracts of the ventricles
- distal (the truncus arteriosus) - the proximal aorta and pulmonary arteries
Four tissue ridges−two each related to the truncus and the conus−develop on the inner aspect of the bulbis cordis. The truncus swellings enlarge and fuse to form the truncus septum, which grows in a spiral course to divide the truncus into distinct pulmonary and aortic channels. The conus swellings also grow and fuse with each other and with the endocardial cushions inferiorly, eventually contributing to the development of the superior portions of both ventricles (including the membranous portion of the interventricular septum). An abnormaly of this complex process is believed to underly the structural components of Tetralogy of Fallot.
Tetralogy is the most frequent anomaly of the conotruncal region, occurring in about 1 per 1000 births. The structural abnormalities which define the condition are: stenosis of the pulmonary outflow tract, a ventricular septal defect and a partially displaced aorta that overrides the septal defect. The latter two abnormalities allow blood to flow from the venous to the systemic circulation. The fourth component of the anomaly−right ventricular hypertrophy−occurs as a consequence of elevated right ventricular pressure. The obligatory right to left shunt typically results in decreased systemic PO2 and cyanosis. Other clinical findings include dyspnea, digital clubbing, syncope (“tet spells”) and embolic stroke (as was likely the case in the 10 year-old boy whose heart is shown here).
Etienne-Louis Arthur Fallot was a French cardiologist who described the condition in detail in 1888. Despite the recognition given to him for this, the anomaly had been documented much earlier by the Danish anatomist Niels Stensen (Nicolas Steno) in 1672, as well as a variety of other physicians in the following years.

